Immuno-Diagnostics Antibodies and Antigens for Parkinson's Disease (PD)
What is Parkinson's Disease (PD)?
Parkinson's disease is a neurodegenerative disorder that primarily affects the motor system. Such a loss of dopamine producing neurons in the substantia nigra region of the brain causes the disease, which results in less dopamine. Dopamine is as important a neurotransmitter as it is to the movement as it is to the emotional responses. These neurons are damaged or killed leading to the characteristic motor and non-motor symptoms seen in Parkinson's disease [1-2].
Pathological Changes in Parkinson's Disease
Parkinson’s disease (PD) involves the loss of dopamine-producing neurons in the substantia nigra, reducing dopamine levels and causing motor symptoms like tremors, rigidity, and bradykinesia. The pathological hallmarks of PD are Lewy bodies, that are protein aggregates based on α-synuclein which impairs the normal functioning of the neurons and causes their death. They are present nearly in all the structures of the brain and are involved in non-motor disorders including memory impairment and mood swings. Owing to decreased serotonin, norepinephrine, and acetylcholine levels, depression, sleep disorders, and autonomic dysfunction occur. These changes emphasise the significance and demand for therapies directed to motor and non-motor symptoms.
Diagnosis of Parkinson's Disease
Parkinson’s disease requires careful diagnosis to diagnose the condition correctly and to rule out other conditions with similar symptoms. Clinical symptom assessment is centered on the documentation of traditional motor abnormality signs such as tremor, rigidity, and akinesia. A neurological examination tests reflexes and coordination, muscle strength, and tone. The drug response test measures the improvement after giving dopaminergic treatments; common a PD symptom. MRI for instance or DaT scan precludes other conditions and evaluates the dopamine transporter. The use of novel biomarker tests such as alpha synuclein, DJ-1, and Neurofilament light chain (NfL) gives relevant information about the diseases anatomic distribution and evolution. This way, integration of these methods provides accurate and comprehensive diagnosis of Parkinson’s disease.
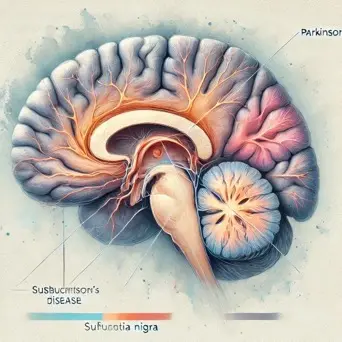
Figure 1. Source: Humain Brain PNG, Vector And Transparent Clipart Images
Validation data
Click to check the technical information for recommended Antibodies:
Beta-Amyloid
Products
- Aβ40/Aβ42
Good performance of GeneMedi's Aβ40/Aβ42 antibodies in ELISA and CLIA Validation
The high-performance Aβ40 and Aβ42 antibody raw materials developed by GeneMedi have the advantages of good specificity and high sensitivity, and are the preferred raw materials for the development of in vitro diagnostics reagents for Alzheimer's disease.
In direct ELISA analysis, GMP-h-Aβ40-Ab01 and GMP-h-Aβ42-Ab01 can Recognizes Aβ40 or Aβ42 with high specificity. GMP-h-Aβ42-Ab02 has cross-reactivity with both Aβ40 and Aβ42.
In CLIA verification, the antibody pair (Capture: GMP-h-Aβ40-Ab01 , Detect: GMP-h-Aβ42-Ab02 ) can detect the GMP-h-Aβ40-Ag01, and the antibody pair (Capture: GMP-h-Aβ42-Ab02 , Detect: GMP-h-Aβ42-Ab01 ) can detect the GMP-h-Aβ42-Ag01. Beta-amyloid(1-42) antibodies (GMP-h-Aβ42-Ab02 and GMP-h-Aβ42-Ab01) established a standard curve, and the detection range of Aβ42 was 100-1700 pg/mL.
Figure 1: Good performance of GeneMedi's Aβ40/Aβ42 antibodies in ELISA and CLIA Validation
A. GMP-h-Aβ40-Ab01 and GMP-h-Aβ42-Ab02 can bind GMP-h-Aβ40-Ag01, while GMP-h-Aβ42-Ab01 can not bind the Aβ40 antigen in direct ELISA.
B. GMP-h-Aβ42-Ab01 and GMP-h-Aβ42-Ab02 can bind GMP-h-Aβ42-Ag01, while GMP-h-Aβ40-Ab01 can not bind the Aβ42 antigen in direct ELISA.
C. CLIA verification data of the antibody pair (Capture: GMP-h-Aβ40-Ab01 , Detect: GMP-h-Aβ42-Ab02 ) to detect the GMP-h-Aβ40-Ag01.
D. CLIA verification data of the antibody pair (Capture: GMP-h-Aβ42-Ab02 , Detect: GMP-h-Aβ42-Ab01 ) to detect the GMP-h-Aβ42-Ag01.

Biomarkers for Parkinson's Disease
| Biomarker | Limit (Pathological concentration in blood) |
|---|---|
| Human Parkinsonism associated deglycase (PARK7) | / |
| Alpha-synuclein (α-synuclein) | >10 pg/ml |
| Tau proteins (Tau) | >10 pg/ml |
| Neurofilament light chain (NfL) | / |
| Glial fibrillary acid protein (GFAP) | / |
| Beta-amyloid 42 (Aβ42) | / |
| Beta-amyloid 40 (Aβ40) | >100 pg/ml |
Sample Types: Blood, cerebrospinal fluid (CSF)




 Full
List Download
Full
List Download